Rectal inflammation is the initial stage of ulcerative colitis, which can then progress to the colon. The symptoms could be intermittent or persistent. Symptoms of these disorders include diarrhea, loss of appetite, abdominal pain, low red blood cell counts, and diarrhea. Although ulcerative colitis cannot be cured, inflammation can be managed with medicine. For more complicated instances, surgery may be a possibility.
Ulcerative colitis: what is it?
Diseases of the inflammatory bowel, also known as IBD, include ulcerative colitis (UC). There is a range of severity in the symptoms. It’s possible that there won’t be any visible indicators at all. The treatment focuses mostly on the management and relief of symptoms.
Diseases of the inflammatory bowel, also known as IBD, include ulcerative colitis (UC). IBD stands for “inflammatory bowel disease,” which is a group of conditions that affect the digestive system.
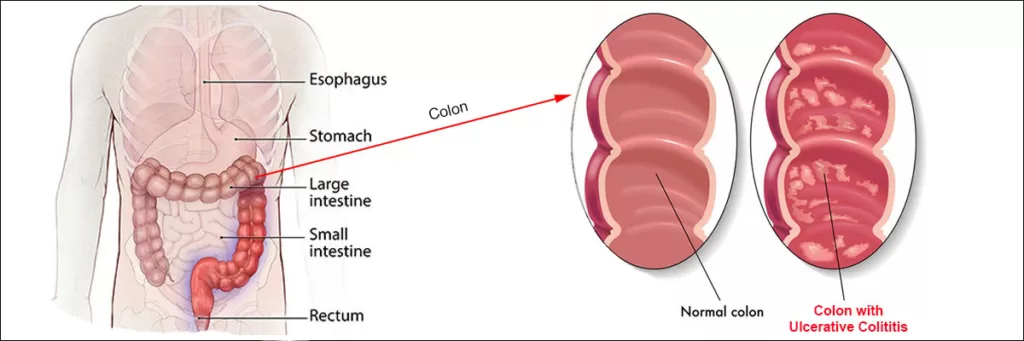
Inflammation of the colon (or large intestine) or rectum (small intestine) lining is what causes UC. The lining of the colon gets inflamed, which causes little sores called ulcers to form. The onset of inflammation is typically in the rectum and moves upward. The entire colon may be affected.
Due to the inflammation, your bowel contents will move quickly and need to be emptied more often than usual. Ulcers develop when cells in the intestinal mucosa die at the surface. Not only could the ulcers bleed, but they could also leak mucus and pus.
Yet, the American Gastroenterological Association says that UC usually starts in young adults between the ages of 15 and 30. There is a little uptick in the incidence of IBD after the age of 50, particularly among men.
Some of the possible contributors to the onset of UC are:
Genes. It’s possible to have UC because of a gene you inherited from a parent.
Several autoimmune conditions Having one form of an immunological illness increases your likelihood of having another. Aspects of the natural world Your immune system can be set off by bacteria, viruses, and other things called antigens.
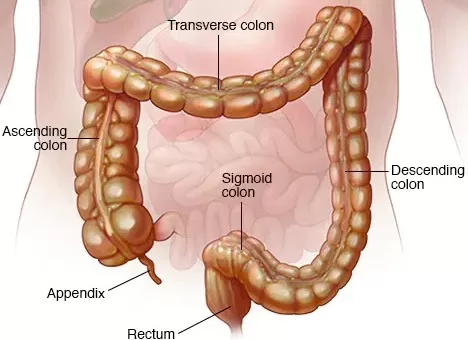
The large intestine, also called the colon, is the part of the digestive system that looks like an upside-down U and is made up of the transverse, descending, and sigmoid sections. Being the last section of the large intestine, the rectum plays an important functional role.
Each section of the large intestine (commonly known as the colon) has a different purpose. Being the last section of the large intestine, the rectum plays an important functional role.
Some common signs that your body conveys having U C
If you have ulcerative colitis (UC), your large intestine may become inflamed and develop ulcers. They classify it with other inflammatory bowel diseases (IBD). It causes severe, urgent diarrhea that frequently includes blood. These symptoms may force you to get up and use the restroom in the middle of the night.
The rectum, which is near the anus, is often the site of the first inflammation in ulcerative colitis (where poop leaves your body). There is a risk that the inflammation will spread and impact the rest of your colon.
Having ulcerative proctitis means that you have inflammation of the rectum and lower intestine. Pancolitis is an inflammation that affects the entire large intestine. Limited colitis, also called distal colitis, is an inflammation that only affects the left side of the colon.
Both the degree and location of inflammation contribute to UC’s severity. Indeed, there is something unique about each and every person. Inflammation in the rectum of the colon, which is a small area, can be severe (large area) or mild (small area).
You may have times when your ulcerative colitis symptoms are at their worst. These are called “flare-ups.” The disease may show little or no symptoms during remission. Remission is the desired therapeutic outcome (in years).
Around 50% of patients with ulcerative colitis have mild cases. Meanwhile, some have persistent temperature spikes, bloody stools, nausea, and stomach cramps. Arthritis, eye inflammation, liver illness, and osteoporosis are just some of the conditions that ulcerative colitis has been linked to.
The cause of these symptoms outside of the colon is unknown. Researchers suspect that inflammation produced by your immune system contributes to these consequences. When the colitis is treated, some of these symptoms disappear.
Even though anyone can get ulcerative colitis at any age, it happens most often between the ages of 15 and 30, with a smaller number of cases between the ages of 50 and 70. One study found that 20% of patients with ulcerative colitis also had a close relative with the condition. Also, it can happen to children as young as 2, and about 20% of all cases are found in people younger than 20.
Difference between ulcerative colitis with regular colitis
Inflammation or irritation of the colon is known as colitis. Several factors, including microbial or viral illness, can contribute to this. Although both Crohn’s disease and ulcerative colitis can last a lifetime, ulcerative colitis is more severe since it is not infectious.
Is ulcerative colitis common?
The gastrointestinal disease ulcerative colitis is surprisingly common. This condition affects up to one in every 250 people in North America and Europe, making it the second most common inflammatory bowel disease after Crohn’s.
The Symptoms of Ulcerative Colitis
The symptoms of ulcerative colitis frequently worsen over time. At first, you might observe:
- Sudden and uncontrollable diarrhea or bowel motions
- Pain in the belly area (abdomen).
- Tiredness.
- Nausea.
- Reducing body fat.
- Anemia (lower red blood cell count) (lower red blood cell count).
- Potential Later Issues
- Bowel movements with blood, mucous, or pus
- Painful cramps.
- Fever.
- Skin reactions or skin irritations
- sores in the mouth.
- Painful joints.
- Irritated, red eyes.
- Liver problems
- Drop in consumption of food and water.
Children with ulcerative colitis have similar signs and symptoms, and their growth may also be slowed down. You should tell your child’s pediatrician about any and all symptoms because some ulcerative colitis symptoms can look like those of other diseases.
How does one go about diagnosing ulcerative colitis?
In order to make a diagnosis of ulcerative colitis in children, teenagers, and adults, your doctor will first need to rule out any other possible causes of your symptoms. If they find anything wrong after a medical examination, they could prescribe:
Your blood can reveal whether or not you have an infection or anemia. A deficiency of iron in the blood is known as anemia. It may indicate internal bleeding in the rectum or colon.
Human feces: There are a number of diseases and conditions that can be detected in one’s feces, including inflammation, infection, and parasites (which are small organisms that can live within a person).
Radiology and other imaging tests: Your doctor may want to see a picture of your intestines and stoma. You might have to go through a series of diagnostic tests, some of which will involve imaging techniques like a computed tomography (CT) or magnetic resonance imaging (MRI) scan.
Your lab technician may run an endoscopy test on the advice of your physician. An endoscope is a thin, flexible tube with a small camera on the end that is used for medical procedures. Specialized doctors can put an endoscope into the anus to look at the rectum and colon. Colonoscopy and sigmoidoscopy are two of the most frequently performed endoscopic examinations.
Who makes the determination that a patient has ulcerative colitis?
Your primary care doctor is likely to send you to a specialist if you present symptoms of ulcerative colitis. Adults need to be under the supervision of a gastroenterologist, a doctor who focuses on the digestive system. The treatment of children and adolescents should be overseen by a pediatric gastroenterologist.
How do doctors manage ulcerative colitis patients?
Even though there is no known cure for ulcerative colitis, it can be treated with medicines that reduce inflammation, improve symptoms, and let people get back to their normal lives. Individualized treatment plans are developed based on the patient’s condition and severity. Medication is the main method doctors use to control the condition.
If diagnostics show that an infection is to blame for your symptoms, your doctor will likely treat the infection first to see whether it improves your condition. Medication for ulcerative colitis is designed to do two things: improve patients’ quality of life and increase the length of time they spend in remission. Different kinds of drugs are used by doctors to reduce inflammation in the large intestine.
In order for the tissue to heal, the inflammation and irritation must first be reduced. It may also help alleviate discomfort and stop diarrhea. Your doctor may suggest the following for infants, kids, teens, and adults. If you have mild to moderate ulcerative colitis, your doctor may suggest an aminosalicylate called sulfasalazine (Azulfidine®).
If you have a sulfa allergy, you should tell your doctor. Instead, you may be given a sulfa-free aminosalicylate like mesalamine (Canasa®, Delzicol®, Asacol® HD, Pentsa®, Lialda®, and Apriso®). Deep inflammation in your colon or rectum can be treated with medications that come in pill and enema/suppository form.
You may need a corticosteroid like prednisone (Deltasone®) or budesonide (Entocort® EC, Uceris®) if your ulcerative colitis is particularly severe. Due to their harmful side effects, doctors tell you not to use corticosteroids for longer than you need to. To keep the patient in remission, other drugs may be employed.
Immunosuppressants such as 6-mercaptopurine (Purixan®, Purinethol®), azathioprine (Azasan®, Imuran®), and methotrexate (Trexall®) are examples. These drugs are useful for reducing the activity of a hyperactive immune system. The biological drugs used to treat severe ulcerative colitis are aimed at certain parts of the immune system.
Is surgery an option for me for U C?
When medical treatments haven’t worked or when problems come up, like bleeding or abnormal growths, surgery may be needed. The formation of precancerous lesions, which can progress into colorectal cancer, is a possibility. A doctor can remove these growths either surgically (through a colectomy) or endoscopically (through a colonoscopy).
Studies show that 30% of people who have ulcerative colitis will need surgery at some point in their lives. In childhood, about 20% of kids with ulcerative colitis will require surgery.
Surgery options for ulcerative colitis include:
The ileoanal pouch and proctocolectomy; Most people with ulcerative colitis choose J-pouch surgery, which includes a proctocolectomy and an ileoanal pouch. There are a few different ways to perform this process, and it usually requires more than one operation. At first, you’ll have a proctocolectomy, in which your colon and rectum are taken out.
The surgeon then makes a new rectum by making a bag out of your small intestine called an ileoanal pouch. It’s possible that your surgeon will also perform a temporary ileostomy while you’re in the hospital getting your new pouch implanted and your body ready for surgery. This makes a hole (stoma) in the patient’s lower abdominal wall. The stoma, a little pink flap of skin, is where your small intestines join your body.
When you’ve healed, your ostomy bag will be linked to your stoma so that you can empty your small intestinal waste into it. Place the tiny bag flat on your outside, just below your waistline. You’ll need to keep the trash bag on your person at all times. The bag needs to be changed several times a day.
The members of your medical staff will instruct you on how to clean the stoma and remove waste from the bag. Even while you’re undressed, no one will be able to tell where your waste is if you use a fabric cover for the pouch. The pouch may be kept odor-free and undetectable under clothing with regular use.
After you and the ileoanal pouch have healed, your surgeon will talk with you about closing the ileostomy.
Stools are still collected in your new ileoanal pouch. This permits normal feces and urine discharge via the anus. Your big intestine can no longer hold all of your waste, so you have to go to the bathroom all the time (on average four to eight times a day once your body has adjusted). But, after the operation heals, you should feel much better. After a while, ulcerative colitis symptoms like discomfort and cramps should fade away.
Colon removal and ileostomy
If your doctors decide that an ileoanal pouch is not a good choice for you, they may suggest a permanent ileostomy (without an ileoanal pouch). In a proctocolectomy, the colon and rectum are surgically removed. At the same time, a permanent ileostomy is created (as described above).
What factors contribute to colitis flares
If you’ve managed to put your ulcerative colitis into remission, you should take every precaution to keep it that way. Some potential triggers include:
Emotional stress: Try to get at least seven hours of sleep every night, stay active every day, and find healthy ways to deal with stress, like meditation.
Instead of nonsteroidal anti-inflammatory drugs (NSAIDs) like Motrin® and Advil®, take acetaminophen (Tylenol®) for pain relief and fever reduction.
If you feel your symptoms have been worsened by antibiotics, be sure to tell your doctor.
The influence of diet and nutrition on UC
Neither eating habits nor a change in diet can prevent or treat ulcerative colitis. However, your or your child’s diet may help with symptom control and extend the time between flare-ups.
Some foods may aggravate symptoms and should be avoided, particularly during episodes of worsening. Each person has a unique set of foods that can bring on their symptoms. Keeping a food diary can help you determine which foods cause reactions by helping you see patterns in your eating habits and post-meal feelings.
Often cited culprits in the realm of unhealthy eating include:
- Foods that are high in fat.
- Sugary foods and beverages.
- Beverages with carbonation.
- Meals that are high in fiber.
- Alcohol.
- High salt intake.
- Dairy foods.
Carefully monitor your kid’s eating and eating habits. During a flare-up, if their appetite goes down, they might not eat enough calories to stay healthy and grow. Ulcerative colitis can cause inflammation in the digestive tract, which can make it hard for food to be absorbed properly. Your child’s health is also at risk. Because of these factors, it may be necessary to boost your child’s caloric intake.
Disclaimer:
This information is for educational purposes only, and no medical advice should be inferred from it. Before changing your diet or adding supplements, please talk to your doctor.
The author’s views are his or her own. The facts and opinions in the article have been taken from various articles and commentaries available in the online media and Eastside Writers does not take any responsibility or obligation for them.






Pingback: The Secret Health Superpower of Ash Gourd: Unlocking the Benefits of Winter Melon for Optimal Wellness - Eastside Writers
Pingback: Uncovering the Secrets of Fig: From Ancient Food to Modern Medicine - Eastside Writers