Emphysema and chronic bronchitis are just two of the many lung diseases that fall under the umbrella of chronic obstructive pulmonary disease, or COPD. Having been diagnosed with COPD raises the possibility that you also have emphysema or asthma, both of which are serious lung diseases.
As COPD gets worse, it gets harder and harder to breathe because air can’t get in or out of the lungs easily. As COPD gets worse, it gets harder and harder to breathe because air can’t get in or out of the lungs easily. Coughing, wheezing, and chest tightness is other common symptoms. direction indicator: up and to the right
Neither the disease nor the damage it causes to the lungs can be cured, but with the right treatment and close cooperation with your doctor, you can slow its progression and manage your symptoms.
COVID-19 can cause a variety of symptoms, including fever and coughing. Pneumonia and respiratory distress can occur in severe cases. Some COPD patients are more vulnerable to severe symptoms after contracting COVID-19. If you have the chronic obstructive pulmonary disease (COPD), preventing illness is even more crucial. In this regard, the vaccination against COVID-19 is an important preventive.
Even people who have been vaccinated might want to wear a mask that fits well when they are in a room with a group of people because people with chronic conditions are still more likely to get serious or severe diseases.
Maintain your regular medication schedule if you are currently treating COPD. If you have any of the COVID-19 symptoms listed above or think you may have been exposed to the virus, don’t be afraid to call a doctor.
What exactly is COPD
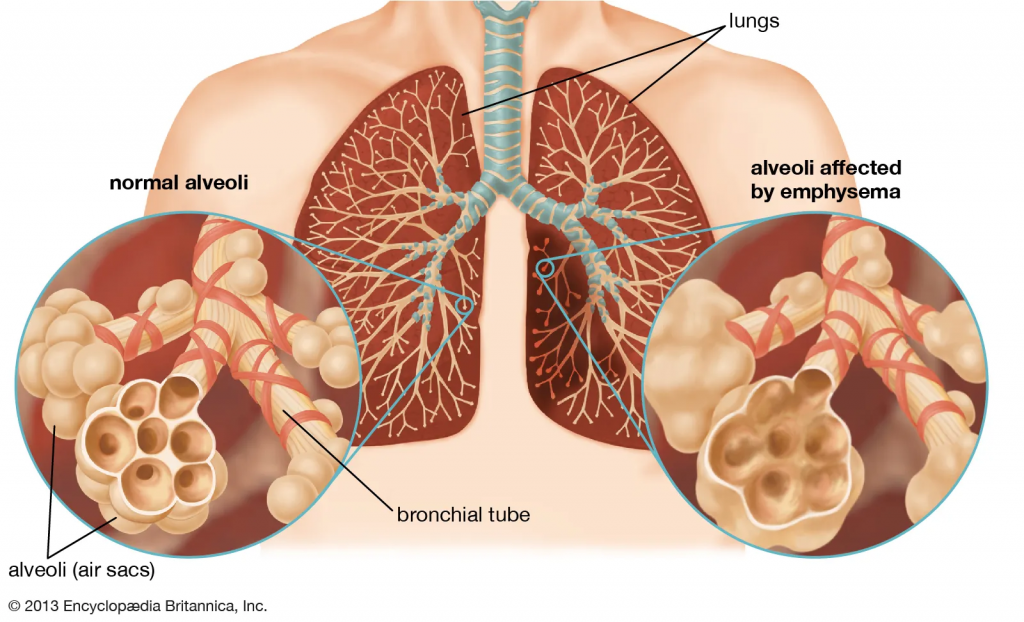
COPD, or chronic obstructive pulmonary disease, is caused by damage to the air sacs in the lungs (emphysema) and inflammation and narrowing of the bronchial airways (chronic bronchitis).
Cigarette smoking is the most common cause of the chronic obstructive pulmonary disease (COPD). Breathing becomes increasingly difficult as lung damage worsens. When the lungs get a lot of damage, it can be harder for them to get oxygen into the blood and get rid of carbon dioxide from the body. A variety of symptoms, including shortness of breath, result from these alterations.
Treating COPD can help manage symptoms like shortness of breath and chronic cough, and in some cases, it can even slow the disease’s progression. However, quitting smoking and staying away from secondhand smoke is the single most effective way to boost your mood.
In this article, we’ll look at how COPD patients can get the care they need. COPD is broken down into its constituent parts: causes, symptoms, and diagnosis.
Take adequate measures to Combat COPD
Those living with COPD can take steps to improve their health and lower their risk of complications by following a few simple guidelines.
The first and most important step in treating COPD is for patients to quit smoking. Regardless of the severity of your illness, this holds true. COPD progression can be slowed by quitting smoking, regardless of how long you’ve had the disease. Quitting smoking can be hard, but your doctor can help you and give you advice.
Infections of the respiratory system can worsen COPD symptoms. Vaccination is a crucial part of COPD management and should not be skipped. Some examples are:
There are two vaccines against pneumococci, one of the most common bacteria that can cause pneumonia (called Pneumovax and Prevnar). Age and other factors determine which vaccinations are recommended. If you’re unsure whether you need both vaccines or just Pneumovax and when you should get them, talk to your doctor (the vaccine may need to be repeated at 5- to 1-year intervals).
The flu shot is recommended every year before flu season starts, which in the northern hemisphere is usually in the fall or early winter.
If you are 19 or older and have never gotten the whooping cough vaccine (pertussis, you should. It is recommended that all adults over the age of 50 get the shingles vaccine because it protects against the disease and the complications that can arise from it. Patients with chronic obstructive pulmonary disease may be more susceptible to shingles.
Protect yourself from COVID-19 with the recommended vaccine for anyone over the age of 12: COVID-19 vaccine. Those who suffer from COPD are more likely to experience life-threatening complications. The landscape of vaccines is always changing, and so is how often you need a booster shot. Talk to your doctor about which vaccinations are right for you and how often you should get boosters.
You may be given antibiotics by your doctor if you end up getting sick with an infection. Antibiotics may be given if your symptoms are very bad or if the doctor thinks you have a bacterial infection. However, antibiotics don’t always work because most respiratory infections are caused by If you think you might have the flu, talk to your doctor. You might need antiviral treatment. be necessary.
Most of the time, it’s not a good idea to take antibiotics every day to prevent infections. If you have frequent flare-ups (two or more per year) despite treatment, your doctor may suggest that you take the antibiotic azithromycin to prevent them.
Eat Well And Stay Fit to avoid COPD
Nutrition: Symptoms of advanced COPD can prevent some patients from eating enough. People with advanced lung disease are more likely to experience unexpected weight loss. Malnutrition, which is caused by not eating enough, can make symptoms worse and make it easier to get sick. If you are not getting enough to eat or are losing weight despite your best efforts, you should consult your doctor.
To up your calorie intake, try these methods:
- The key is to eat frequently and in small amounts, but make them of nutrient-rich foods (such as eggs)
- Simplify your diet by eating ready-made meals (for example, microwaveable meals)
- Relax before eating.
- Take a multivitamin every day.
- Take vitamin and mineral supplements (drinks or bars that contain a lot of calories and nutrients)
- If your doctor suggests it, take an appetite stimulant.
On the flip side, being overweight can exacerbate COPD symptoms. If you’re worried about losing weight too quickly, your doctor can help.
COPD patients should see their doctors on a regular basis for monitoring as part of their treatment plan. Your doctor will ask you about your symptoms, how well your treatments are working, and if you have any other health problems that could be making your COPD worse. Even though each patient’s situation and health will ultimately determine how often they go to the doctor, it is safe to assume that they will go every few months or more.
Medication for Chronic Obstructive Pulmonary Disease
Along with the general measures we talked about above (see “General measures”), medication therapy is an important part of treating COPD. Depending on the type and severity of your symptoms, your doctor may give you one of the medications listed in Table 1.
Along with the general measures we talked about above (see “General measures”), medication therapy is an important part of treating COPD. mucus production in the lungs.
Inhalers:

Mainstaydose inhalers (MDIs), dry powder inhalers (DPIs), soft mist inhalers (SMIs), and nebulizers are all common ways to inhale bronchodilators (a device that turns liquid medication into a fine mist that you breathe in).
Most people rely on inhalers. In order to get the right amount of medication into your lungs, using an inhaler correctly is crucial.
Bronchodilators
Various bronchodilators are available. “Short-acting” medications provide rapid symptom relief and are prescribed for use as needed.
SABAs
Short-acting beta-agonists (SABAs), which are also called “rescue inhalers,” can help people who are having trouble getting enough air quickly.
SAMAs
Anticholinergics, or short-acting muscarinic antagonists (SAMAs), are used to treat respiratory conditions by relaxing the muscles in the airways. A SAMA that is taken as needed may be recommended if your symptoms are mild and infrequent. Since SABAs work faster than SAMAs, doctors usually choose SAMAs, unless the SABAs make the patient feel jittery or give them a fast heart rate.
The action plan
An inhaler with both a short-acting beta agonist (SABA) and a long-acting beta agonist (SAMA) can be used sometimes or all the time, depending on what the patient needs for their symptoms.
Over time, “long-acting” bronchodilators help keep symptoms at bay. Medications have their own individual dosing and administration schedules that come with the package (for example, once daily or twice daily).
The long-acting medications currently available for the treatment of COPD are:
Extended-release muscarinic receptor blockers
Anticholinergics, or long-acting muscarinic antagonists (LAMAs), help people with chronic obstructive pulmonary disease (COPD) breathe easier and experience fewer episodes of shortness of breath. If your symptoms aren’t being managed by treatments like short-acting bronchodilators, your doctor may suggest trying a long-acting muscarinic antagonist (LAMA).
Long-acting beta agonists (LABAs) may be given to you if other medicines don’t help you control your symptoms.
When a single drug isn’t enough to treat the symptoms, doctors often give a combination of LAMAs and LABAs. When it is convenient, you can use a combination inhaler to take all of your medications at once, or you can use your regular inhalers for each of the medications.
A class of medications known for their anti-inflammatory effects is called glucocorticoids. Steroids, corticosteroids, or even just steroids are common names, but these are not the same substances as those used by some athletes to bulk up. Glucocorticoids can be administered in a variety of ways, including by inhalation, oral consumption, and intravenous administration (a thin tube that goes into a vein).
If your symptoms are not under control with a long-acting bronchodilator alone, or if you have frequent exacerbations, you may want to consider using inhaled glucocorticoids for long-term symptom control. There are several combinations like this, and one inhaler combines an inhaled glucocorticoid with a long-acting beta-agonist (LABA) and a short-acting beta agonist (LAMA)
COPD flare-ups are usually treated for a short time with glucocorticoids, either orally (in the form of a pill) or intravenously (through a needle) (glucocorticoids given through an IV are done in the hospital). Due to the fact that they could have bad effects, however, they are usually only used for short periods of time.
Medication for chronic obstructive pulmonary disease
drugs like roflumilast and theophylline are reserved for patients whose COPD symptoms persist despite standard treatment.
People with chronic cough and phlegm production (chronic bronchitis) who have frequent flare-ups even though they regularly use inhaled bronchodilators and glucocorticoids may be given the oral drug roflumilast. (For more on this, see “Bronchodilators” and “Glucocorticoids”)
A pill called theophylline has been shown to help with shortness of breath in some people. As a result of its negative effects, it sees limited use.
Some patients may benefit from taking azithromycin, an antibiotic that has been shown to lessen the severity and frequency of flare-ups.
Cough suppressants are not recommended for people with COPD. Even though a cough is annoying, trying to stop it with medicine could make you more likely to get an infection.
COPD Accompanying Treatments
Quitting smoking (if you smoke) is the most important of the general measures that everyone with COPD should take. Other than medication, there are treatments that can help alleviate symptoms and boost the quality of life that doesn’t involve taking anything.
Low blood oxygen levels are a common complication of advanced COPD. Even if you don’t notice any symptoms, the condition known as hypoxemia can still be present. Either a finger-clipped device (a pulse oximeter) or a blood test can determine how much oxygen is present in the blood (arterial blood gas). Hypoxemia patients can get oxygen therapy, which has been shown to help them live longer and have a better quality of life.
Oxygen therapy
A cannula is a small tube that is put into a person’s nostrils and connected to an oxygen tank or machine in their home. All of these things, as well as when and how to clean and replace them, will be demonstrated to you by your healthcare provider.
If you smoke, you should never use oxygen supplements. Due to the fact that oxygen can catch fire, smoking while using it can cause severe burns. People using oxygen tanks have died in accidents where they tried to light up.
Changes in cabin pressure during flight may increase the risk of hypoxia for passengers with chronic obstructive pulmonary disease. If you are at risk for hypoxemia, your doctor may give you a bottle of oxygen to take with you on an airplane.
Endobronchial valves
Endobronchial valves are small devices that are put into the airways using a bronchoscope, which is a tube that is put down the throat through the mouth or nose. The diseased area can vent its air, but fresh air can’t get in. This allows the stronger, healthier sections of the lung to carry a greater burden during breathing. EBVs may help people with emphysema whose symptoms keep coming back even after medical treatment and pulmonary rehabilitation.
Surgical procedures
Some people with advanced emphysema find relief from their symptoms through surgical procedures like lung volume reduction surgery or lung transplantation.
The goal of lung volume reduction surgery is to improve the patient by removing the most severely damaged portions of lung tissue. For those who have tried everything else for their symptoms, including pulmonary rehabilitation, this may be a last resort.
Unfortunately, not everyone will improve after surgery, and some may even get worse. A doctor might suggest a CT scan or another imaging test to help figure out how likely it is that this treatment will help.
Lung transplant
In severe cases of COPD, a lung transplant may be an option. Transplantation, if successful, may alleviate symptoms. The life expectancy of COPD patients has not been shown to improve after lung transplantation.
The Prediction of Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) usually gets worse over time, but the way it gets worse and how long a person lives are both very hard to predict (your prognosis). How well your lungs perform during exercise, how much you continue to smoke, and whether or not you have any other health issues are all factors in how severe your COPD symptoms will be. Those with COPD who have milder symptoms, maintain a healthy weight and don’t smoke have a better prognosis than those who don’t.
Clinicians use tools like the “BODE index” to figure out how likely a patient is to live and when it would be best to do a lung transplant. Body mass index (BMI), spirometry airflow obstruction severity, exertional dyspnea severity and six-minute walk distance are all factors in the calculation. Your doctor can use the calculated number to better assess your prognosis.
What is progressive COPD?
Patients, family members, and medical staff should not avoid talking about death and dying, even though it can be difficult to bring up the subject. This is especially true for those who are dealing with a life-threatening illness like COPD.
Ahead-of-time care planning: COPD doesn’t always mean death. However, it is important to begin discussing your wishes for the end of your life long before you are in a terminal condition. When it comes to end-of-life decisions, such as whether or not to use a ventilator (a breathing machine) when natural breathing becomes impossible, people’s values and preferences vary widely. Share your feelings about this with those closest to you.

The Alternatives
Palliative care: Palliative care is a term for treatments that aim to alleviate symptoms and improve quality of life rather than cure or halt the progression of a disease. Palliative care is useful for people with COPD not just at the end of life but at any time. Treatments for breathing difficulties, cough, fatigue, insomnia, anxiety, depression, and pain are all part of palliative care.
Opioids, like morphine, may be given to people with COPD whose severe symptoms are no longer helped by standard treatments. In some cases, noninvasive ventilation is used to help a patient breathe.
Hospice care: Hospice care is sometimes suggested for people who have less than a six-month life expectancy. All of the patient’s and family’s needs, including those of a physical, mental, emotional, social, and spiritual nature, must be addressed.
Hospice care is provided by a team that may include a physician, registered nurse, nursing aide, chaplain or religious leader, social worker, and volunteers and may take place in a patient’s home, a nursing home, or a hospice facility. Hospice care is a difficult experience for everyone involved, but having support and assistance ceases the load.
Disclaimer:
The author’s views are his or her own. The facts and opinions in the article have been taken from various articles and commentaries available in the online media and Eastside Writers does not take any responsibility or obligation for them.
Note: Contact our Writers at www.eastsidewriters.com for writing Blogs/Articles on any niche. We have experts in various domains from Technology to Finance and from Spirituality to Lifestyle and Entertainment.







Pingback: Why CoQ10 Is The Drug Of Choice For Many When It Comes To Health Management - Eastside Writers
Pingback: The Deadly Truth: Smoking And Its Effects on Human Organs and Mortality - Eastside Writers